 Uncovering disparities in breast cancer screening and opportunities for intervention
Uncovering disparities in breast cancer screening and opportunities for intervention A new study reveals a noticeable 38% of eligible women in commercially insured health plans are skipping critical breast cancer screenings, a rate higher than the national average. The greatest gaps in screening rates are observed among the socio-economically disadvantaged and in certain geographic regions, highlighting the need for targeted interventions to increase awareness and access to screenings. Summary
Enterprise Analytics Core domain(s): health equity/SDOH, HEDIS, oncology
Background
Timely breast cancer screening is critical in early disease detection and has been shown to effectively increase survival rates. The American Cancer Society (ACS) recommends that women aged 45-54 years should undergo annual mammography, whereas those aged 55-75 should participate biennially. This guidance has been reinforced in the Healthcare Effectiveness Data and Information Set (HEDIS) reporting for breast cancer screening, which is utilized by the National Committee for Quality Assurance (NCQA) to measure the performance of health plans. Understanding health inequities or disparities in breast cancer screening will help identify sub-group of health plan members requiring targeted interventions.
Objective
To assess disparities in breast cancer screening among eligible members enrolled in commercial health plans.
Methods
The Healthcare Integrated Research Database (HIRD®) was used to identify commercially enrolled women aged 45 to 64 years with continuous coverage in the years 2020-21. Members were excluded if they had a diagnosis of breast cancer or underwent diagnostic mammography in 2019. Eligible members were identified to have undergone breast cancer screening if they had a medical claim for mammography as identified using the CPT or HCPCS codes in either 2020 or 2021. To understand disparities, the proportion with no screening was assessed by age, region, and social drivers/determinants of health (SDOH) measures, and flagged as disparity if the proportion differed from the overall non-screening rate by >5%.
Results
2.1 million commercially insured women were eligible for breast cancer screening in 2020 or 2021 based on inclusion criteria. Below are some key observations on breast cancer non-screening rate:
Figure 1. Zip codes with at least 50% or above non-screening rate in 2020-21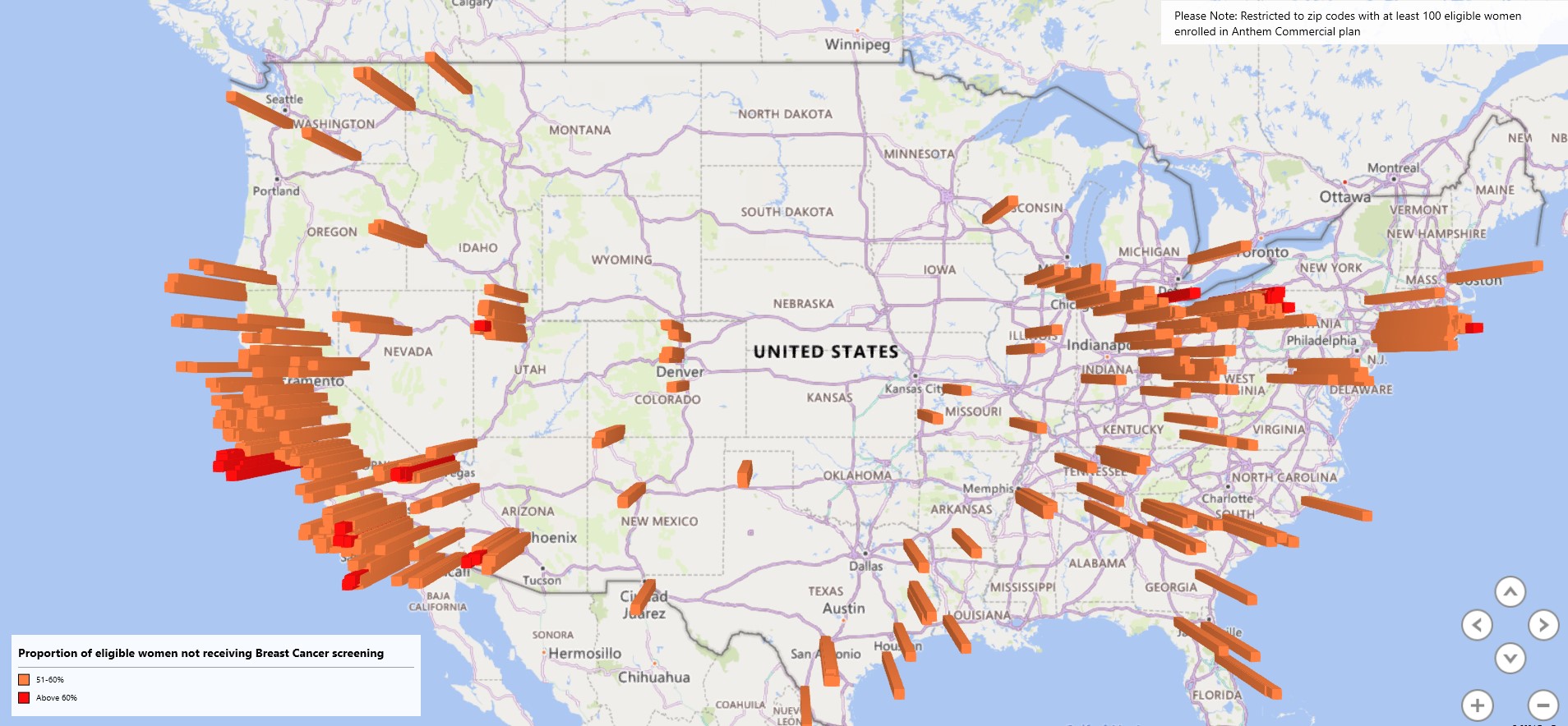
Key takeaways
^CarelonRx and Carelon Research collaborated with a manufacturer to deploy programs that raise awareness about the importance of screenings to providers in communities identified by the methods above. The impact of these targeted interventions through these collaborative efforts will be evaluated.
Carelon Research project team: Nilesh Gangan (PI), Shivani Pandya*, Aaron Haynes, John Barron, Jay Visaria
*Carelon Research associate at the time of the study.
For more information on a specific study or to connect with the Actionable Insights Committee,
contact us at [email protected].
Sponsor: Carelon Research conducted this study in collaboration with CarelonRx. Dissemination and sharing of the Newsletter is limited to Elevance Health and its subsidiaries and included findings and implications are for Elevance Health and its affiliates’ internal use only.
Lorem ipsum dolor sit amet, consectetur adipisicing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut.

"Et harum quidem rerum facilis est et expedita distinctio!"

"Nam libero tempore, cum soluta nobis est eligendi."

"Temporibus autem quibusdam et aut officiis debitis!"